'Profiteering, cold-hearted' nursing home owners should be investigated, congressman says
Letitia Stein reporting project on nursing homes was completed under the auspices of the USC Annenberg Center for Health Journalism’s 2021 National Fellowship.
Other stories by her include:
4 key things to know about USA TODAY’s investigation into nursing home failures during COVID-19
This nursing home chain stood out for nationally high death rates as pandemic peaked
White House ready to crack down on nursing homes, cites USA TODAY report
Guide to nursing homes: How to choose the right home for a loved one in three steps
When does a nursing home COVID-19 death count? It's complicated.
USA Today
A USA TODAY investigation has traced a string of casualties back to one nursing home chain, Trilogy Health Services.
Hannah Gaber, USA TODAY
By Jayme Fraser and Nick Penzenstadler
Corrections & clarifications: An earlier version of this story incorrectly characterized the Indiana attorney general's actions.
In a biting letter, U.S. Rep. Bobby Rush, D-Ill. urged Congress to investigate the failures of nursing homes during the pandemic, particularly “profiteering, cold-hearted” corporations that act as landlords in the industry.
“It is up to Congress … to shine a bright light on the current practices, to reign them in, and to set and strictly enforce high standards for performance,” Rush wrote to the chair of the House Oversight Committee. “It is Congress’s job to stand in-between greedy corporations and those who are the most defenseless.”
The request cited a USA TODAY investigation into nursing home ownership webs invisible to consumers and regulators. The reporting focused on one large operating chain that has an unusual financial partnership with its real estate investors.
Rep. Bobby Rush, D-III., has called for an investigation into nursing home performance during the pandemic. Here, in 2020, Rush spoke at a news conference on Capitol Hill about the "Emmett Till Antilynching Act," which became law earlier this week. J. Scott Applewhite
In a report released this week, the National Academies of Sciences, Engineering, and Medicine called for federal officials to expand the government’s tracking and regulation of nursing home companies.
Increased scrutiny of nursing homes comes as the White House prepares to use executive authority to tighten industry regulations. Those proposals include setting the first nationwide minimum staffing requirements and expanding regulatory authority to crack down on corporate owners with track records of poor performance.
When USA TODAY investigated COVID-19 deaths at the country’s largest nursing home chains during the deadliest peak of the pandemic, Trilogy Health Services stood out for reporting the highest death rate to the federal government, twice the national average. The company filed a revision to reduce its official count of COVID-19 deaths by more than 40%, but its rate remains one of the highest among large chains.
During the pandemic, COVID-19 made its way into most nursing homes in America. Carlie Procell, Ramon Padilla, USA TODAY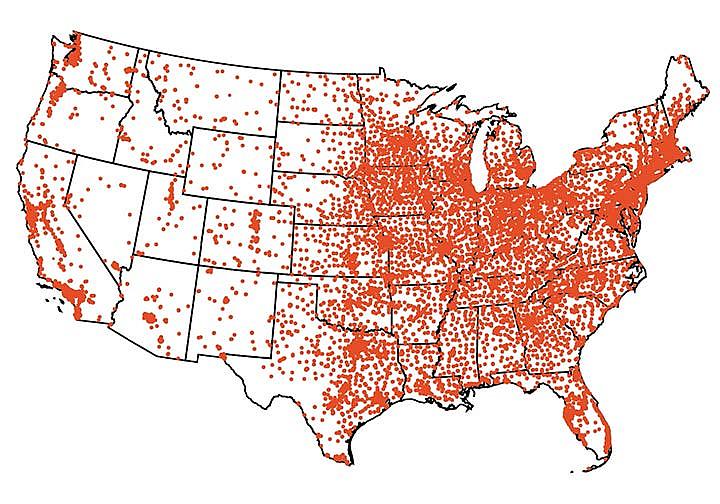
In Indiana, one of four Midwest states where Trilogy operates nursing homes, Attorney General Todd Rokita said in a statement that “the families of those who are affected deserve answers.” His office is reviewing Trilogy and other health systems' reporting and he has asked the state health department to supplement that review.
“I hope the Indiana Department of Health will lead that effort and audit the data it received from hospitals and health care providers,” he wrote.
Officials from that department did not respond to questions from USA TODAY, but spokeswoman Megan Wade-Taxter said in a statement that its staff and partners worked “throughout the pandemic to ensure the data presented to Hoosiers is accurate and timely.”
Indiana Attorney General Todd Rokita is reviewing COVID-19 death reporting by Trilogy Health Services. Doug McSchooler, The Indianapolis Star
A majority of Trilogy’s buildings in Indiana, Kentucky, Michigan and Ohio are owned by a real estate investment trust, American Healthcare REIT. In addition to collecting rent, American Healthcare shares profits from Trilogy's operations – a model allowed under a federal law revised in 2008.
This arrangement could yield more profits in good times but exposes the company to more financial risks, which could create incentives to cut back on care. Rush told USA TODAY that REITs should not be allowed to own nursing homes and collect profits from their operations. The veteran congressman has for years advocated for more staffing at nursing homes to increase the quality of care.
“If they own the real estate, then they should not be given the authority to run or operate these nursing homes and shouldn’t be getting one red cent of the taxpayer’s money in operating these nursing homes,” Rush said, calling it the duty of Congress to “draw the line in the sand.”
House Oversight Chair Rep. Diana DeGette, D-Colo., shares Rush’s concerns, said spokesman Ryan Brown, and has asked Frank Pallone, D-N.J., to add it to the agenda of the Energy and Commerce Committee.
REITs are a financial vehicle for real estate investments that are exempt from corporate income taxes, like mutual funds, as long as most income is paid out to investors as dividends. The concept has become another way to make money from health care, following a trend of private equity firms buying up dental chains and hospital mergers driving up pricing.
Typically, REITs are landlords that collect rent from companies operating inside its buildings. Since 2008, a law passed by Congress has allowed health care REITs to profit from operations inside their property as well.
The concept was permitted earlier for REITs outside health care to allow them to offer basic services for their properties, such as cleaning. American Healthcare REIT appears to be the first large trust to use RIDEA, or the REIT Investment Diversification and Empowerment Act, in nursing homes.
A USA TODAY analysis of ownership data compiled by the Centers for Medicare and Medicaid Services, which regulates nursing homes, reveals how little federal officials know about REIT involvement with nursing homes.
That data reveals only about 500 facilities nationwide as being owned by one of the major, publicly traded REITs or American Healthcare, which is not publicly traded. By contrast, USA TODAY has identified about 1,800 such facilities – one in nine nursing homes.
American Healthcare had the highest reported death rate among seven large REITs during the coronavirus surge of late 2020 and early 2021, according to USA TODAY’s analysis of COVID-19 data nursing homes were required to report weekly. That analysis looked at operating chains and at the REITs that own many of their facilities.
American Healthcare was one of three REITs with a reported death rate above the national average during the weeks reviewed, and Trilogy’s revisions dropped it only one notch, to second-highest.
Photos of some of the 800 people who died at nursing homes operated by Trilogy Contributed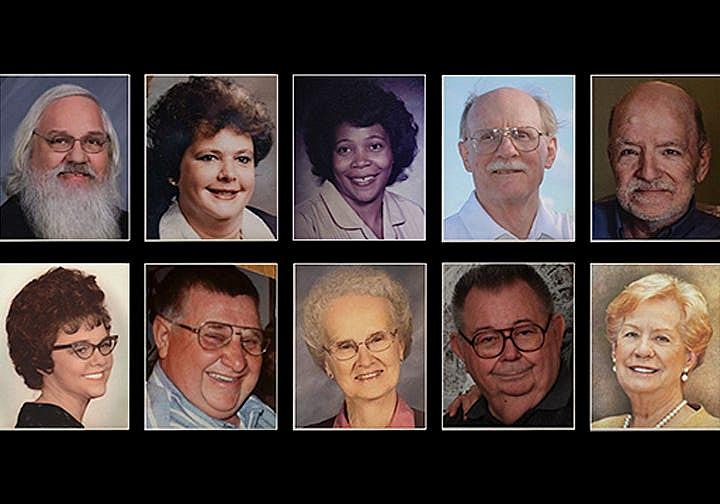
Trilogy declined to identify specific reasons for its deletions of deaths since USA TODAY published its investigation, which appears on the public CMS website. U.S. nursing homes averaged 3.3 deaths per thousand residents each week from October 2020 through February 2021. Trilogy's initial reports revealed seven deaths per thousand residents, and its revised figures show 3.9 deaths per thousand.
Representatives of CMS and the Centers for Disease Control and Prevention, which manages the COVID-19 database, told USA TODAY they are not reviewing the changes to the self-reported data, which nursing homes can correct at any time.
Damon Elder, a spokesman for Trilogy Health Services and American Healthcare REIT, declined a request to speak with company officials about the review in Indiana and the call for a congressional hearing looking at nursing home ownership.
The industry association representing both for-profit and nonprofit nursing homes, the American Health Care Association, said it supports efforts to improve the quality of care but questions some of the suggested changes. Lobbying by the group could complicate efforts to pass changes that require congressional approval.
Public records show the group spent $3.7 million on lobbying the federal government in 2021 with a team of 46 lobbyists. It ranked third in the hospital and nursing home sector behind the American Hospital Association and Children’s Hospital Association, according to reports compiled by OpenSecrets.
LeadingAge, which represents nonprofit homes, spent less than $200,000, according to lobbying disclosure reports. Lisa Sanders, a spokesperson for that group said its members “support initiatives to increase clarity around nursing home ownership and operations.”
The larger association dismissed the potential impact of changes that focus on particular business models or expand regulatory oversight to include corporate owners. The group argued the focus should be on increasing Medicaid reimbursement rates for care and upping other federal investments.
“It is the lack of adequate government support for long term care that policymakers should be examining,” the association said in a statement. “Because of this public policy failure, some nursing homes have been forced to look for other private investment opportunities in order to keep their doors open.”
Academic researchers and the National Academies’ report note that savvy corporate owners can use a variety of related businesses to draw money out of nursing homes. An individual facility may appear unprofitable to federal regulators even as an owner higher up the corporate chain earns profits. Financial moves can help companies minimize their taxes and shield money from potential lawsuits but make it difficult for governments to understand how the tax dollars spent on care are used.
How many nursing homes are unprofitable is unknown, researchers said.
Ashvin Gandhi, a UCLA health economist who studies private investment in nursing homes, said it is difficult to know which changes will improve the quality of nursing home care because the government does not have a complete understanding of the business structures and financial incentives that drive decisions.
“It is an extremely important part of the health care system that serves some of the most vulnerable populations,” he said. “It’s important that given the extremely large public investments we make in this care that we understand what we’re buying with our money.”
CMS officials told USA TODAY this year that they evaluate nursing home performance only at the facility level and do not track outcomes by operating chain or the tangle of business interests involved in real estate or services.
“We are actively looking to improve,” said Jonathan Blum, principal deputy administrator at the CMS, said in January.
In its new report, the National Academies urged federal officials to expand the government’s tracking and regulation of companies that own nursing homes and their properties “to avoid a repeat of the failures that occurred during the COVID-19 pandemic,” according to a news release.
“Publicly available ownership information needs to reflect and capture the complexity of today’s nursing home sector,” the report said.
Budgets for staffing, supplies and other needs often are set by corporate owners rather than individual nursing homes, which might limit the impact of regulating at the facility level. The National Academies report suggests that expanding CMS’ regulatory authority to include the corporate chain might make enforcement more effective.
Betty Ferrell, who chaired the committee that wrote the report, said the U.S. nursing home system is “ineffective, inefficient, fragmented and unsustainable.”
Ferrell, director of nursing research and education at City of Hope Medical Center, called for action, saying, “We must stop viewing nursing home residents as ‘them’ – they are our grandparents, parents, friends, siblings and veterans.”
Jayme Fraser and Nick Penzenstadler are reporters on the USA TODAY investigations team. Contact Jayme at jfraser@gannett.com, @jaymekfraser on Twitter or on Signal at (541) 362-1393. Nick can be reached at npenz@usatoday.com, @npenzenstadler on Twitter or on Signal at (720) 507-5273.
[This article was originally published by USA Today.]
