This nursing home chain stood out for nationally high death rates as pandemic peaked
Letitia Stein reported this story while participating in the USC Annenberg Center for Health Journalism’s 2021 National Fellowship.
Other stories by her include:
4 key things to know about USA TODAY’s investigation into nursing home failures during COVID-19
White House ready to crack down on nursing homes, cites USA TODAY report
Guide to nursing homes: How to choose the right home for a loved one in three steps
When does a nursing home COVID-19 death count? It's complicated.
Dying for care: How nursing homes failed during COVID-19
'Profiteering, cold-hearted' nursing home owners should be investigated, congressman says
cdf4.jpg?itok=VauGthCj)
Martha Miles, one of the first to die, gasped for air. She pressed her nursing home call buzzer but got no help.
Ed Windholtz, Imelda Balbach, Byron Eggemeyer – farmer, nurse, engineer – died hundreds of miles apart within the span of a week in seemingly isolated COVID-19 outbreaks.
The deaths across a scattering of Midwestern nursing homes began surging around Thanksgiving. In the span of a week, the count of the dead nearly tripled in Michigan. Then residents started dying by the dozen in Ohio and Indiana. By Valentine’s Day last winter, the death toll had climbed into the hundreds.
AUSA TODAY investigation has traced the casualties back to one nursing home chain, Trilogy Health Services, owned by a real estate venture with a new business plan for the cutthroat world of elder care.
The deal promised a historic investment opportunity, then delivered the highest death rates reported by any large nursing home chain at the height of the pandemic.
Residents at Trilogy’s 115 campuses died of COVID-19 last winter at twice the national average for nursing homes, USA TODAY found, based on figures facilities must file weekly with the federal government.
Presented with USA TODAY’s findings, the company said it had mistakenly reported hundreds of deaths during the surge. Trilogy offered a revised tally that would reduce its COVID-19 death count by more than 40%. The company declined to provide documentation needed to vet those claims but said Wednesday it had filed new numbers with the federal government.
Even by its own drastically lower numbers, Trilogy’s death rates still would have ranked well above the national average for nursing homes during the winter surge.
Until now, such pervasive failures escaped notice. In a first-of-its-kind analysis, USA TODAY has revealed ownership webs invisible to consumers. Problems across chains eluded federal officials overseeing nursing homes, who were focused on individual facilities during the pandemic.
Reporters scored the performance of every nursing home in America to probe questions of corporate responsibility left unanswered by dozens of research papers on COVID-19’s more than 140,000 nursing home deaths.
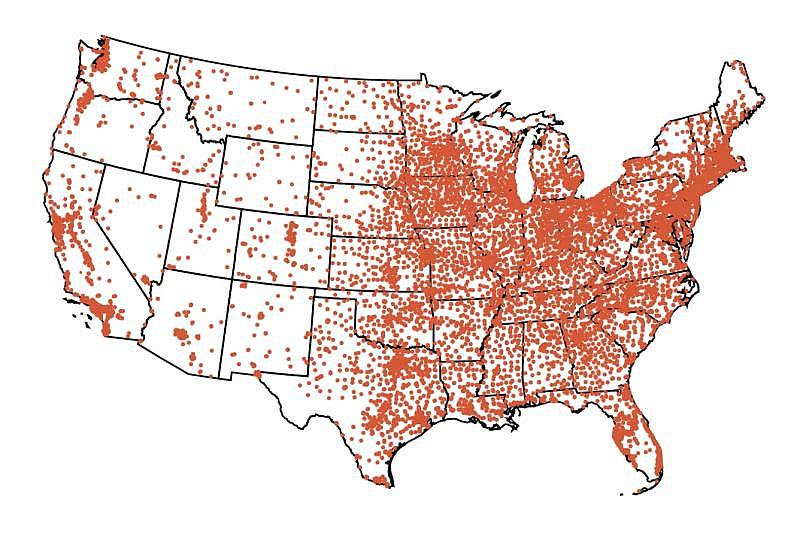
How U.S. nursing homes fared during COVID-19’s worst surge
Trilogy's outcomes did not appear to be driven by residents who were older, or more fragile, factors accounted for in USA TODAY's analysis.
Its track record cannot be explained solely by its presence in states hard hit by COVID-19, either. If anything, academic studies on the spread of the coronavirus suggest Trilogy’s smaller nursing homes should have been safer.
Trilogy had another unusual distinction from the start. A company specializing in real estate acquired it in a test of a business model new to a large nursing home chain.
The financial pressures coming from the industry’s real estate landlords clearly need more scrutiny, said Ashvin Gandhi, a UCLA health economist who studies private investment in nursing homes, noting that such business arrangements can “affect people’s life and death.”
“It really tells us that we need to know a lot more about what is going on in nursing homes,” he said.



Bethany Pointe, St. Andrews and Waterford Place health campuses are all Trilogy Health Services facilities in Indiana that reported COVID-19 outbreaks during last winter's surge.HANNAH GABER, USA TODAY
USA TODAY spent the past year comparing COVID-19 infection rates, deaths and staffing levels reported by nursing homes. Reporters reviewed thousands of pages of safety inspections and financial materials. They conducted more than 100 interviews with current and former Trilogy staff, family members who lost loved ones at its homes and industry and financial experts. The review found:
- Trilogy went further than any other major chain in shrinking care hours delivered to residents before the pandemic. By the time the pandemic started, a typical resident in a Trilogy home was receiving about 45 minutes less care daily from nurses and bedside aides than the federal government recommends.
- Half of Trilogy’s facilities were cited by health inspectors for violating COVID-19 safety rules in 2020, the first year of the pandemic. Among the lapses written up: nursing aides who dispensed eye drops, lifted patients to the toilet and fed them – all without properly cleaning their hands.
- Trilogy’s poor COVID outcomes stood out by measure after measure. In three of the four states where it operates — Indiana, Michigan and Ohio — its death rates eclipsed those of other large chains with a major presence. In Kentucky, where Trilogy has 13 facilities, it ranked second. The company's revised figures would not change those standings.
- Even as deaths rose, millions of dollars continued to flow from Trilogy to a California-based real estate venture busy preparing its next investment pitch – a stock listing expected to launch this year.
USA TODAY first shared its findings about Trilogy’s high death rate with the company in December, then in January provided detailed information about the analysis, including how the company compared to other large chains. Last month, after being presented with an extensive summary of the investigation’s findings, Trilogy said its self-reported figures were wrong.
The company declined repeated interview requests to discuss the data discrepancies for publication or to provide information in a form comparable to its original filings. Then, CEO Leigh Ann Barney addressed the issue in a video message sent this week to the “Trilogy family,” noting her expectation that the company would be the focus of a forthcoming national media investigation.
“At Trilogy, we took the most conservative approach to reporting, which included non-confirmed COVID deaths,” she said. Barney highlighted how Trilogy also posted COVID cases and deaths on its corporate website for much of the pandemic and described its communications as providing “a level of transparency not found at other long-term care companies.”
“Reporting practices in several of the states where we operate have recently come under scrutiny, specifically regarding under-reporting of cases and deaths,” she said. “Therefore, we feel any comparison data with our competitors at this point is unreliable.”
She cited confusion and changing guidance around what Trilogy had to report and said it had hired a consultant to help it review its death count. Nursing homes can file corrections at any time.
Dying for care: How nursing homes failed during COVID-19(4:23)
A USA TODAY investigation has traced a string of casualties back to one nursing home chain, Trilogy Health Services. HANNAH GABER, USA TODAY
In two interviews last year, executives from Trilogy and its real estate owner discussed their general operations. They highlighted how the company swiftly adapted to the pandemic with new protocols such as separating the healthy from the sick on its campuses.
“We were a leader in doing the things that needed to be done to treat our residents and employees in the safest manner possible,” Barney told USA TODAY in September.
After learning of USA TODAY’s analysis, federal nursing home regulators said they need to collect better information about real estate ownership models like Trilogy’s.
"We are actively looking to improve," said Jonathan Blum, principal deputy administrator at the Centers for Medicare and Medicaid Services, in a January interview.
Last week, President Joe Biden proposed reforms that would track problem owners across states and shed light on how Wall Street profits from nursing homes.
Coming out of the winter surge, the president and CEO of the real estate venture behind Trilogy was offered a compensation package worth millions in stock awards and $1.5 million in salary and a potential cash bonus, records show.
His salary and cash alone could have paid a year’s wages of nearly every nurse and bedside aide at Bethany Pointe Health Campus, according to financial reports that nursing homes submit to the government. This was the Trilogy home in Anderson, Indiana that first demonstrated how the company would handle a pandemic.
Martha Miles died after going to Bethany Pointe in early 2020 to recover following a fall. One night, the 70-year-old had called her son crying, “I can’t breathe.”
Her purse and new pajamas were dumped in an oversized bag in the foyer, he said, before her family learned what went wrong from a notation in her death certificate: “CORONAVIRUS.”
Miles, formerly a social worker, raised three boys and spoiled 18 grandchildren. She died before meeting three of her six great-grandchildren.
Nearly two years later, her son, Marvin Miles, still misses the smell of her pot roast and candied yam dinners. He teared up to learn from USA TODAY about the investment strategy behind the nursing home run by Trilogy.
“They are making money off people’s lives,” he said.
A portrait of Martha Miles sits on a bookshelf in her home. She died at 70 on March 30, 2020 after going to Bethany Pointe to recover from a fall. HANNAH GABER, USA TODAY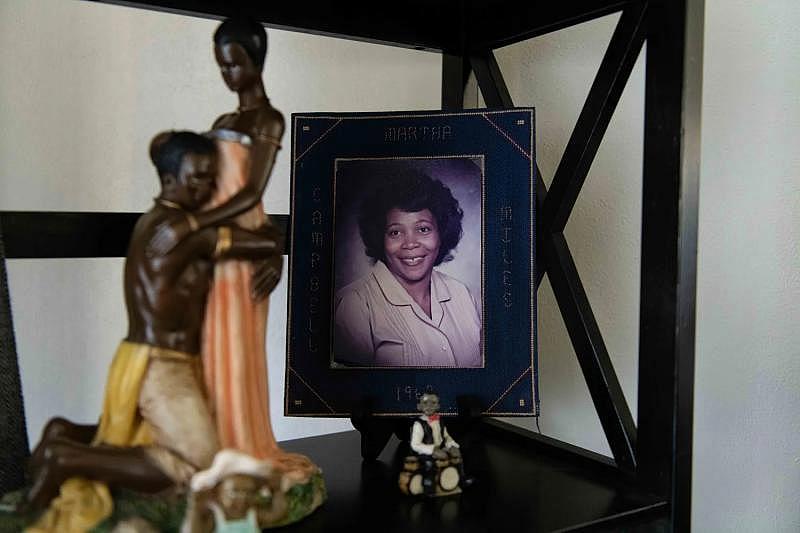
THE BUSINESS MODEL
Danny Prosky, Jeff Hanson and Mathieu Streiff live a world away from the chain of small Midwestern nursing homes, in spacious, multimillion dollar Orange County, California, homes replete with whirlpool baths, architectural pools and panoramic views.
The trio has worked together for years building real estate investment portfolios. In an interview, Prosky recalled how they bailed in late 2011 from a sponsoring firm headed into bankruptcy. To safeguard an investment, he said they shut down on a Friday and by Monday had relaunched with new support.

Financial filings with the U.S. Securities and Exchange Commission in June 2021 by the real estate venture behind Trilogy.SEC
Their expertise is Real Estate Investment Trusts, known as REITs. These companies can own most any property that generates rent. Buying shares of REIT stocks lets individuals invest in large properties, from office buildings to the land under cell towers.
REITs are exempt from corporate income taxes, just like mutual funds, so long as most of their income gets paid out to investors in the form of dividends. The concept has become yet another way to make money from health care, following a trend of private equity firms buying up dental chains and hospital mergers driving up pricing.
In 2015, Prosky and his team led the REIT purchase of a majority stake in Trilogy. The $1 billion acquisition of the growing nursing home chain doubled the size of their portfolio, which was targeting the future needs of a booming senior population known as the “silver tsunami.”
Until Trilogy, major nursing home operators and their REITs had separated the real estate from the care delivered inside. But Trilogy wasn’t for sale under that kind of arrangement, Prosky told USA TODAY.

How to choose a nursing home in 3 steps
So the REIT purchased not only Trilogy’s properties, but also the health care operations inside its campuses. The approach meant a chance at bigger profits – as well as more risk in an economic downturn.
“This was an operator of real estate that we wanted to be associated with,” Prosky said.
Nursing homes looking to boost profits have limited options. The business is heavily subsidized by government-funded health care programs for seniors and people with disabilities. Improving relationships with local hospitals, for example, can shore up more referrals, industry insiders say.
One approach is cutting staff costs, typically half of the operating budget in nursing homes, said Tyler Braun, an assistant professor at Cornell University studying health economics.
“It is ultimately going to have effects on patient care and quality,” he said.
"PRESSURE BUILT UP"
Administrators who ran individual Trilogy facilities said they never heard from the California landlords, but several recalled years of tight budgets and an increasingly competitive culture that ranked facilities by business performance metrics.
“That pressure built up,” said Jessica Trinko, former executive director at The Heritage in Findlay, Ohio, who now works at a non-profit nursing home.
In the years after the REIT takeover, staffing cuts became the norm, USA TODAY found in its review of federally filed expense reports. Paid hours per resident for nurses and aides, a figure that includes sick leave and vacation, fell by 13% over four years at facilities Trilogy currently operates. By contrast, nursing homes nationally cut 2% on average in that timeframe.
The cuts did not play out evenly. As of early 2020, Trilogy’s registered nurses provided slightly more care hours than most large chains, although the levels still fell one-third below recommended federal minimums. These nurses are trained to assess medical conditions and matter the most in how the government rates nursing homes on quality.
Trilogy’s staff reductions targeted a different category of caregiver. At facilities operated by Trilogy, staffing of certified nursing assistants, called CNAs, fell to among the lowest levels of major operators. These frontline caregivers feed and bathe residents, help them to the toilet and change diapers, and make sure they do not get bed sores.
“CNAs are the foundation,” said Charlene Harrington, professor emerita at the University of California, San Francisco, who has studied nursing home quality for over four decades. Without sufficient staffing, she noted, “the work just doesn’t get done. It’s impossible.”
CNAs at Trilogy, including trainees and medication technicians, had about two hours a day to spend with each resident when the pandemic started, according to data submitted to the government from nursing home timesheets. Recommendations from a 2001 federal study urged close to three hours at a minimum.
The author of that study, Vanderbilt University Center for Quality Aging Director John Schnelle, reviewed USA TODAY’s analysis of Trilogy’s CNA staffing levels during the pandemic. He called the staffing hours “awful,” “terrible,” “abysmally low.”
You don’t even have time to take somebody to the bathroom, much less take all the steps that you need to prevent infection spread.
-John Schnelle, Director of the Vanderbilt University Center for Aging Quality
“You don’t even have time to take somebody to the bathroom, much less take all the steps that you need to prevent infection spread,” he said.
The pandemic left CNAs harder pressed for time with sicker patients while juggling new requirements to guard against the spread of infection. Gowns and gloves had to come on and off constantly. More handwashing. Shifting public health guidance on the use of masks. Patient interactions could take twice as long.
Asked about its years of cuts, Trilogy provided USA TODAY with figures that showed far higher staffing levels – some of the best among large chains. The difference? Trilogy included the hours logged by nurses for administrative duties.
A recent academic review of three dozen major studies on nursing homes during the pandemic later suggested that having a larger staff increased the odds of COVID-19 entering a nursing home. But once the virus got in, more care could keep residents alive.
At Trilogy, people started dying.
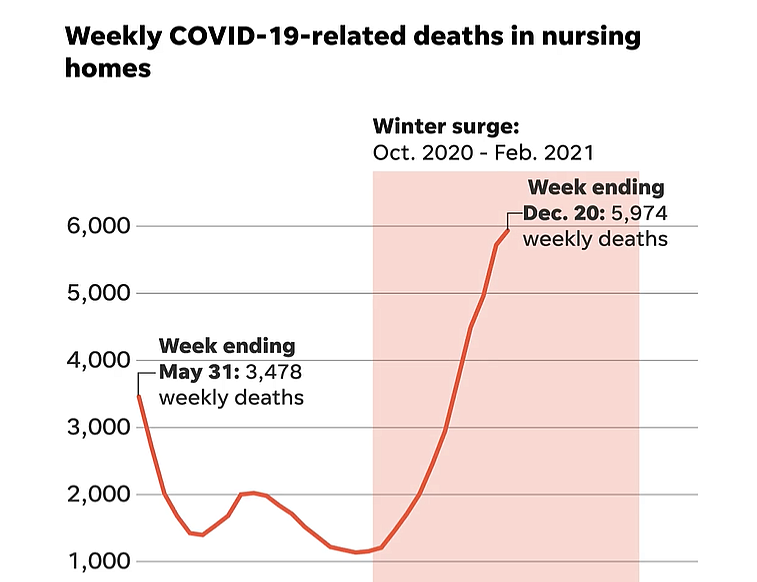
Despite established public health protocols on how to protect nursing home residents, COVID-19 deaths climbed during the winter surge to their highest recorded levels since federal reporting began in May 2020.
Infections and deaths declined once vaccines became widely available, but by then more than 71,000 residents had died from COVID-19-related illnesses during the deadliest peak.
COVID-19 DANGER ZONES
Trilogy’s COVID-19 game plan called for dividing campuses into red, yellow and green zones to limit exposure to the virus. Eyewitness interviews and the reports filed by health inspectors indicate this safety regimen was often a charade.
A Trilogy facility in Battle Creek, Michigan, cordoned off a “red zone” by hanging a plastic wall on one side of a hallway, a December inspection report showed, but did nothing to block off the other end beyond putting a sign on a table that read “no entry.”
Doors were left wide open to the COVID-19 patients’ rooms, state health inspectors found. Aides didn’t know how long to wipe down equipment for proper sanitation. Soon all but two residents were infected. According to its reported figures, 21 residents died.
As winter started, infection swept through Cobblestone Crossings Health Campus in Terre Haute, Indiana, earlier cited for failing to enforce proper hand cleaning. Workers fell sick from the kitchen to the laundry to the bedside. Eighteen residents died.
Remembering the pandemic’s nursing home victims
Natalie Hornback, a former aide there, recalls feeling powerless. “There wasn’t anything we could do,” she said.
An outbreak in Kokomo, Indiana, lasted nine weeks and infected 88 residents at Trilogy’s Waterford Place Health Campus. By the end of January, 29 had died.
Overnight, the facility turned into a scene from a sci-fi movie, with plastic barriers and bins set out for discarded masks and gowns. CNA Nicole Steele remembers feeling shocked, then her work routines turned into chaos.
She recalled sick and frantic residents “on their lights constantly” calling for help.
Showers used to come before breakfast. But in COVID-19, she had to wash residents in bed. Doing that right could take 45 minutes. Two nurses and two aides on some days had to cover residents on three hallways, she said. Mornings passed in a blur of trying to deliver bites of breakfast off trays wrapped in plastic.
By the time you’re done, it’s lunch time. You couldn’t get people fed completely.
-Nicole Steele, CNA at Trilogy’s Waterford Place Health Campus
“By the time you’re done, it’s lunch time,” Steele said. “You couldn’t get people fed completely.”
Frustrated and emotionally spent, Steele posted a remembrance on Facebook to a patient who died from COVID-19, an action she says led her to be fired for violating patient privacy. Asked about it, Trilogy officials declined to comment on an employee’s situation. They also denied reporters permission to visit several of the company’s hard-hit campuses.
In early December 2020, Waterford resident Sue Miller ran a 103-degree fever, her only COVID-19 symptom. Two weeks later, a hospice nurse called, urging relatives to come fast. The facility was on lockdown, but they could say their final good-byes.

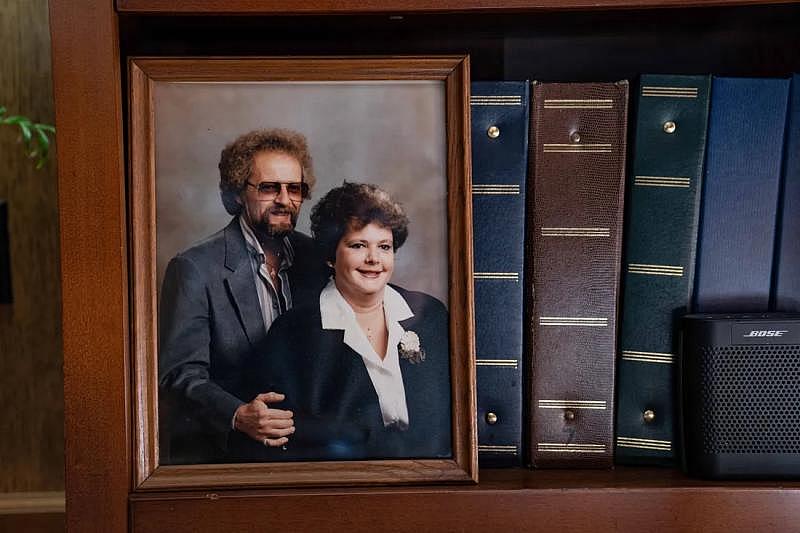
Shana Driver and her relatives were allowed inside during an active COVID-19 outbreak at Waterford Place Health Campus in Kokomo, Indiana for a deathbed vigil for her mother, Sue Miller, whose photograph with her husband now sits on a shelf in Driver's home.HANNAH GABER, USA TODAY
Four of Miller’s children, their spouses, a granddaughter and a niece were allowed inside, one at a time, each for 15 minutes, according to a daughter, Shana Driver. They weren’t questioned when they stretched their permitted visits into a four-day, round-the-clock deathbed vigil.
The first day, they were given masks, face shields, gowns and gloves. They rarely saw staff after that, Driver said. No one checked their temperatures or refilled the box of gloves they had quickly used up in the entryway of a standalone building designated the red zone.
Inside, Driver said they saw a nurse slip her mask down at Miller’s bedside. Staff touched Miller without gloves. A nurse went to her car and back without changing her gown. Used masks, gloves and gowns eventually spilled out of the entryway trash.
“I don’t know that they had a clue what they needed to do,” said Driver, who felt guilty removing her mask briefly for a kiss and sliding off her own gloves to rub cocoa butter lotion into her mom’s arms.
Miller, 77, died with family by her side in a cold, beige room on a Monday, four days before Christmas. Her holiday tree was still in a box.
Shana Driver keeps the ashes of her mother, Sue Miller, and father, Charles Miller, and ornaments made in their memory at her home outside Kokomo, Indiana. HANNAH GABER, USA TODAY
Her family had not been notified when health inspectors documented COVID-19 violations. In November, state inspection reports show, an aide got caught chatting at a nursing station with a mask down. Multiple staffers needed training on how properly to put on and take off gowns.
A later inspection in January found a resident without a mask wandering from room to room in the memory care unit, finally grabbing a used mask from the trash. The same resident earlier had roamed freely with a 101-degree fever and then a dry cough.
Waterford Place ended up with more than $20,000 in fines, while its reported death rates spiraled.
TRILOGY STANDS OUT
COVID-19 marched into almost every nursing home in America during last winter’s surge, when 71,000 residents died – the most of any wave of the pandemic. Still, at more than a quarter of the nursing homes reporting outbreaks, no one died.
USA TODAY’s analysis adapted a statistical model created by the federal government to assess how well nursing homes controlled COVID-19 infections and deaths. Reporters also calculated average death rates from information that facilities reported weekly under federal mandate to ensure uniform COVID-19 tracking across the nation’s nursing homes.
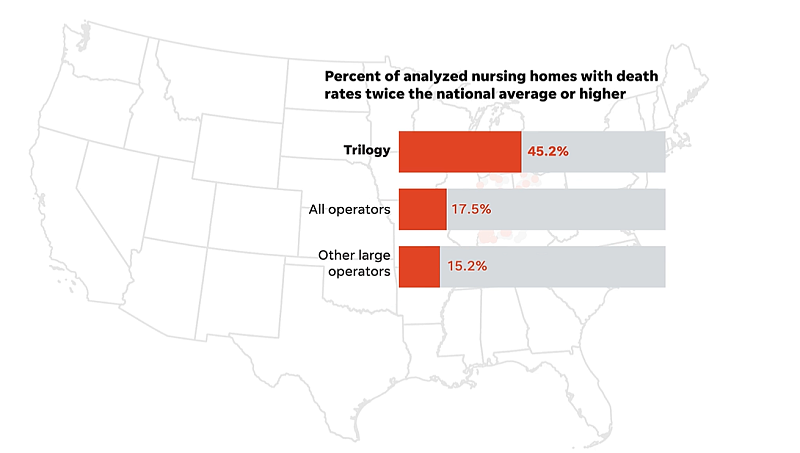
Over and over, Trilogy stood out compared to other major national chains based on its own reports to the federal government. Here’s one example of how Trilogy emerged from the pack:
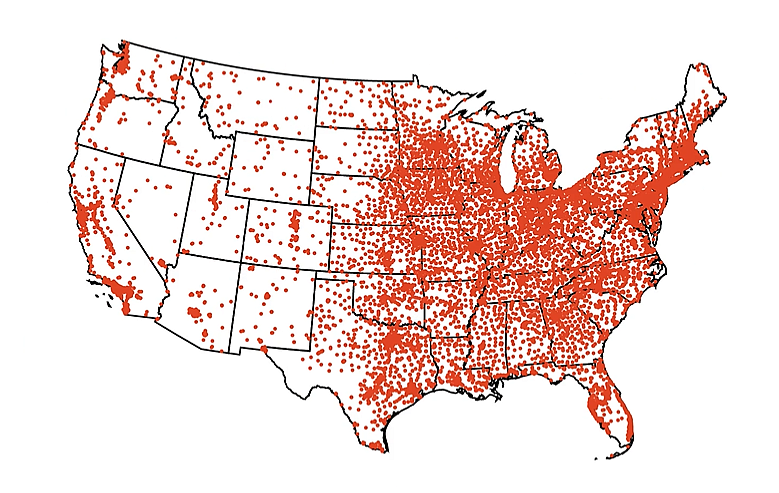
USA TODAY started by looking at the nation's more than 15,000 nursing homes to see which had reported the most COVID deaths during that peak a year ago.
To find systematic problems, reporters set aside small operators and focused on facilities owned by the nation's biggest chains.
That left 1,674 nursing homes.
To find the chains that reported the most deaths to the federal government, USA TODAY first narrowed the field to nursing homes with COVID-19 infections or deaths during the winter surge.
Then to homes with death rates above the national average.
Then to those whose own data showed death rates twice the national average, leaving 283 of the nation’s deadliest big-chain facilities.
Of those, one owner stood out – Trilogy Health Services – with 47 facilities with high death rates based on its weekly reports to the government.
Trilogy operates 115 nursing homes in the U.S.
Of the 104 Trilogy homes with adequate COVID-19 data, 45% had death rates double the national average, the company’s filings showed.
No other major chain had a higher share of its facilities on the list of nursing homes with high death rates.
Responding to these findings, Trilogy now says it mistakenly overcounted hundreds of COVID-19 deaths in reports to the government.
Not all Trilogy homes were among the nation’s worst; based on the company's original filings, 17 of them had no deaths during the surge. But the chain overall stood out for how often people died once they became sick. In all, the chain reported 772 COVID-19 deaths last winter.
U.S. nursing homes averaged 3.3 deaths per thousand residents each week, while Trilogy's initial reports revealed 7.0 deaths per thousand. The new figures provided by Trilogy to USA TODAY are not detailed enough to allow a precise comparison. However, Trilogy’s revisions would appear to put its death rate about 40% above the national average, still ranking it among the highest for leading chains.
After spending weeks reviewing USA TODAY’s findings, Trilogy responded with a written statement in which its CEO, Barney, called the government data “demonstrably unreliable and incorrect.”
“Trilogy has always made residents our top priority, and our caregivers are health care heroes having worked day and night to preserve the safety and health of seniors in our facilities,” she said in the statement.
Barney referenced a report from the U.S. health department’s inspector general, which examined the early days of the federal reporting. At the time, there were news reports of errors at individual facilities. The report found the vast majority of nursing home submissions appeared complete. An updated OIG evaluation is due to be published this September.
By last winter’s wave, facilities had been reporting COVID-19 deaths and cases to the federal government for months. The data has been used extensively by researchers. Health regulators relied on it to monitor and respond to hot spots in real time.
The federal public health office working with nursing homes on the weekly surveys said it had not heard of a large chain needing to make a correction that would eliminate hundreds of previously reported deaths.
USA TODAY was unable to substantiate Trilogy’s explanation for reporting 318 deaths that it now says should not have counted. The company failed to respond to requests for detail and documentation of the reasons. Nor did Trilogy provide its revised counts at the facility level as required for the government database, the National Healthcare Safety Network (NHSN).
“Recently, as a result of the inquiry by USA TODAY, Trilogy performed an internal audit of its NHSN reporting and engaged an independent third-party firm to review the results of the internal audit in order to ensure accuracy,” a company statement said.

When does a nursing home death count?
USA TODAY did its best to examine Trilogy’s concerns. For instance, the company noted that it operates in four Midwest states that had high levels of community transmission during the winter surge.
This was already accounted for in USA TODAY’s analysis. Because academic research on COVID-19 consistently linked outbreaks in nursing homes to the level of virus in the county at large, USA TODAY drilled down into the counties where Trilogy operates nursing homes. Reporters found its communities had 15% higher infection rates than the nation while Trilogy’s original reported death rates were 112% greater than the national average.
Trilogy told USA TODAY another issue in its reporting involved confusion between nursing home residents and those receiving assisted living services on the same campuses. But the limited breakdown provided by the company of its assisted living deaths represented a small fraction of the total Trilogy says it incorrectly reported.
Other factors that Trilogy cited – such as duplicate reporting or residents who tested positive for COVID-19 but died from other causes – either did not hold up upon further review, or could not be validated by USA TODAY.
Trilogy’s reported numbers do show, however, that the chain rapidly refilled its beds as the virus raged on. Trilogy reported 204 deaths over two weeks in December 2020 but its resident population only dropped by 99.
On Facebook, Trilogy advertised a move-in special at many of the facilities battling outbreaks. “Hurry in,” it wrote. “Offer ends soon.”
THE DEAD
Emergency calls from a dozen Trilogy facilities at the height of the winter surge show how people’s final moments played out: He’s hypoxic, turning purple … Screaming, respiratory distress … Dry-heaving, pulse elevated, shortness of breath … He’s a hot mess … Fighting with the family all day on code status, there’s not much we can do.
In conversations with USA TODAY Network reporters, families who lost loved ones at Trilogy facilities grieved for lives cut short and the loss of final good-byes.
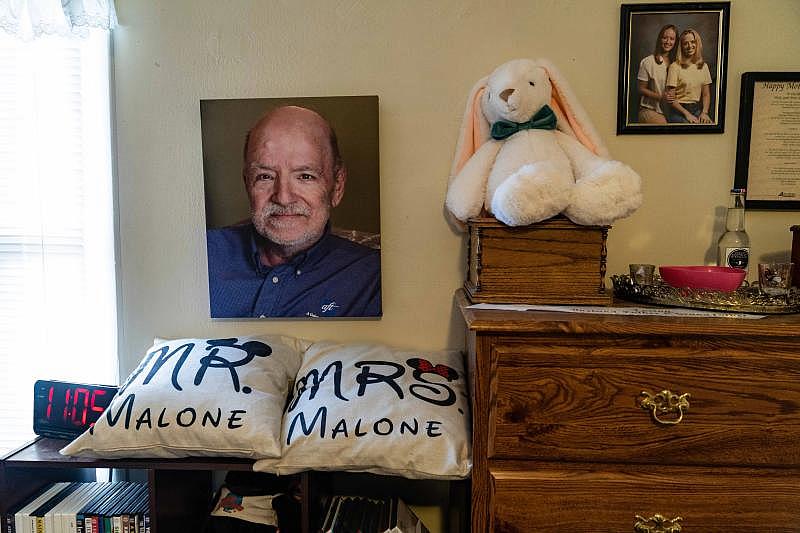
Those who died at the start of the pandemic, such as 65-year-old Bill Malone, never made the federal government’s official count because reporting was not yet required. Malone, a community theater star, went to a Trilogy facility in Anderson, Indiana, to recover after a heart attack. He died without his wife by his side.


Carlynn Malone keeps mementos of her husband, Bill, close at hand. She had a blanket made from community theater T-shirts collected by her husband, who died in the Bethany Pointe care facility at 65 in an early COVID-19 outbreak. Malone also had a necklace made from his wedding ring.HANNAH GABER, USA TODAY
“I did not get to talk to him,” said his wife, Carlynn Malone, who still sleeps with an oversized stuffed gorilla to fill his empty spot in the bed. “I wanted to say ‘I love you.’”
Ann Clay, 78, was a quiet intellectual who preferred quilting and reading to socializing before developing dementia. When the pandemic prevented her husband from visiting in person, he felt reassured to see staff wearing masks and gowns in the background of their Zoom calls.
Ron Burgess, 71, and John Kline Jr., 73, died in early December in an outbreak at a Trilogy facility in rural Ohio. Burgess, a former nurse, for years had put his flowing beard to use as the town Santa in Bellville, Ohio. Kline’s wife of 47 years snuck him a milkshake during their final visit.
Phyllis Thompson, a minister’s wife enjoyed piecing together 1,000-piece jigsaw puzzles. She died on her fourth day in COVID-19 isolation at a Trilogy facility in Louisville, Kentucky.
Ed Windholtz, 83, liked to tell dirty jokes. He was a farmer and lifelong bachelor with eight sisters, and selected the Trilogy facility where he died in Batesville, Indiana for its Catholic name. His surviving sisters remain heartbroken that friends couldn’t attend his funeral.
Imelda “Mel” Balbach, 89, a retired nurse, quickly declined after she tested positive for COVID-19 at a Trilogy facility. She died during an outbreak during which her Evansville, Indiana nursing home reported that half of residents infected with COVID-19 died.
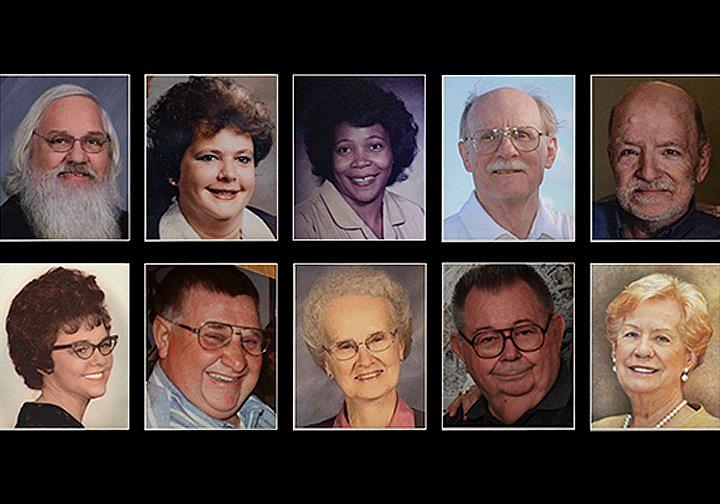
Here are the stories of 14 Trilogy residents who died
Reba Hammons, 96, baked lemon meringue pies before dementia eroded her quality of life. Her daughter, Sharon Williams, praised the vigilance of workers at her Trilogy home in Battle Creek, Michigan, against a virus running rampant. “They tried very hard,” she said.
Byron Eggemeyer’s daughter worried but could do little more. She spent their final visit shivering outside his window at a Trilogy nursing home in Terre Haute, Indiana. The 87-year-old former engineer – “Boppy” to his grandchildren – could barely open his eyes as she held up a photo of a newborn great-grandchild that he would never meet.
In her father’s obituary, Brenda Weeks purposely wrote that he died of COVID-19 while living at Cobblestone Crossings Health Campus.
“I was mad then, and I’m still mad now,” she said. “I was shaming them.”


Brenda Weeks' father, Byron Eggemeyer, died of COVID-19 last winter while residing at Cobblestone Crossing Health Campus in Terre Haute, Indiana. She says her grandson looks like her father, at the same age.HANNAH GABER, USA TODAY
HISTORIC STOCK LISTING
The real estate venture behind Trilogy came out of the winter surge with cash on hand and planning underway for its next business move. What is today called American Healthcare REIT proposes a major stock offering. It touts a now-$4 billion portfolio as potentially “the largest healthcare REIT listing in history.”
Trilogy is central to the pitch. “Trilogy was our best performing manager before COVID hit,” Prosky, the CEO, said on a call with investors last summer. “They've had the best recovery so far in 2021.”
A 158-page annual REIT financial report from the pandemic’s deadliest year for nursing homes contains many facts and figures. It does not detail the chain’s COVID-19 death toll.
It shows that Trilogy’s share of the company reported $107 million in net operating income, a metric used to gauge profitability. That includes revenue from resident fees and services, as well as federal COVID-19 relief, minus property operating expenses.
This view of financial performance does not break down nursing home income from that contributed by independent and assisted living services on the same campuses. Skilled nursing accounts for more than half of Trilogy’s business, REIT officials said in an interview.
Prosky highlighted the financial challenges of the pandemic and noted that government aid saved its bottom line in 2020.
“I would by no means call it a healthy year,” Prosky said.
The REIT reported, under its Trilogy business segment, receiving $53.9 million in federal COVID-19 relief. Multiple REITs involved in its complex ownership arrangement benefited, according to filings with the U.S. Securities and Exchange Commission. A minority REIT stakeholder, NorthStar Healthcare Income, said its share was $12.5 million.
USA TODAY provided officials with American Healthcare REIT with details from its analysis and written questions and asked for further discussion around the complex financial statements. AHR offered no response beyond referring to its SEC filings. Northstar did not respond to inquiries emailed to company officials and media representatives.
David Grabowski, a health care policy professor at Harvard University medical school who studies nursing home performance, said USA TODAY’s findings underscore the need for greater transparency about ownership and financial accountability.
“Places can’t just siphon off dollars,” he said. “They actually have to put those dollars back into direct patient care.”
Financial filings required of REITs offered insight into how corporate chains and REITs can make money off Medicare and Medicaid, the federal health insurance programs for seniors and people with disabilities.
The nursing home industry’s corporate layers can result in individual facilities posting losses while investors profit off their parent companies, according to attorney Ernie Tosh, who maintains a national database of nursing home financial information used by other lawyers filing lawsuits for families and prosecutors fighting fraud.
“That is why people die,” Tosh said. “The facilities would rather take that profit than staff correctly.”
That is why people die. The facilities would rather take that profit than staff correctly.
-Ernie Tosh, attorney
The stock listing proposed for later this year involving Trilogy will explore Wall Street’s appetite for using a federal law known as RIDEA, or the REIT Investment Diversification and Empowerment Act, in a big nursing home chain.
Since 2008, this law has enabled health care REITs to make profits from operations beyond collecting rent on real estate. The concept was permitted earlier for REITs outside of health care to allow them to offer basic services for their properties, such as cleaning.
A possible upshot, experts say, is better collaboration between a landlord and the tenant, who together figure out how best to run the businesses inside their property. That model is commonly used in assisted and independent living.
Still, Trilogy’s arrangement puts a REIT in the business of running a large nursing home chain delivering life-and-death care, industry insiders said.
“When you get into personal care and health care, there can be a slippery slope,” said Stephanie Krewson-Kelly, author of the industry guide Educated REIT Investing, who helped review USA TODAY’s analysis of Trilogy’s REIT profitability.
During COVID-19, this model would have left a REIT on the hook for “the financial implications of unfortunately a lot of death, and certainly a lot of illness in the four walls of the facility,” said Rich Anderson, a senior Wall Street analyst who covers the industry for investment firm SMBC Nikko Securities America.
The concept, by law, requires an independent manager to oversee the health care operations inside the REIT’s properties. But the lines appear blurry.
The REIT behind Trilogy focuses on “buy and sell” real estate and development decisions, general counsel Gabe Willhite told USA TODAY.
“Making sure that you’re on track on budget and understanding how the performance is going is important to everybody here, so those are the things that we focus on a lot,” he said.
Employees and the day-to-day operations fall to a management entity led by Trilogy’s CEO, Barney, who described seeking approval from the parent company for longer-term plans.
In separate interviews with officers from the REIT and Trilogy, USA TODAY was told the REIT also closely watched COVID-19 numbers.
Sabra Health Care REIT, traded on the NASDAQ stock exchange, prefers a landlord role with nursing homes. In a typical industry arrangement, its nearly 300 nursing homes sign leases agreeing to rents that can increase each year by 2% to 2.5%.
CEO Rick Matros said he would not consider RIDEA for a health care business as complex and regulated as nursing homes.
“All of a sudden,” he said, “you have direct responsibility for what happens there.”
Letitia Stein reported this story while participating in the USC Annenberg Center for Health Journalism’s 2021 National Fellowship. This report was also supported by the Economic Hardship Reporting Project. Jeff Kelly Lowenstein is the Padnos/Sarosik Endowed Professor of Civil Discourse at Grand Valley State University.
The team behind this project
- Reporting Letitia Stein, Jayme Fraser and Nick Penzenstadler, USA TODAY, with freelancer Jeff Kelly Lowenstein
- Contributing reporters Aleszu Bajak, Nathan Bomey, Elena Durnbaugh, David Heath, Thomas B. Langhorne, Dean Narciso, Briana Rice, Deborah Yetter
- Editing Amy Pyle and Steve Suo
- Photo and video Hannah Gaber, Jasper Colt, Chris Powers, Emily Johnson, Liz Dufour
- Graphics Carlie Procell, Ramon Padilla
- Digital production Chris Amico, Mara Corbett, Ryan Marx, Annette Meade, Kyle Omphroy, Reid Williams
- Social media and engagement Nicole Gill Council, Teresa Lo
[This article was originally published by USA Today.]
