Reporter Frank Gluck recently spent five months reporting on how Alzheimer’s disease has affected Southwest Florida, where the population of seniors is twice the national average. Here he shares some essential reporting lessons and tips for others tackling the topic in their region.
Health Insurance and Costs

New research from Berkeley economist Ben Handle finds that one company's health care spending dropped 17 percent after switching to high-deductible plans. The research gives new insight into how people's health care habits change when the incentives shift.
_0.jpg?itok=11eAUOo-)
Radio reporter Veronica Zaragovia of KUT in Austin focused her reporting series on the rollout of the ACA in Texas, especially some of its unanticipated effects. Here she reflects on a few of the lessons she learned along the way.
As the media takes stock of the ACA on its five-year anniversary this week, the White House on Wednesday announced a new network of more than 2,800 health care leaders tasked with leading the nation towards a more efficient, less costly model of paying for care.
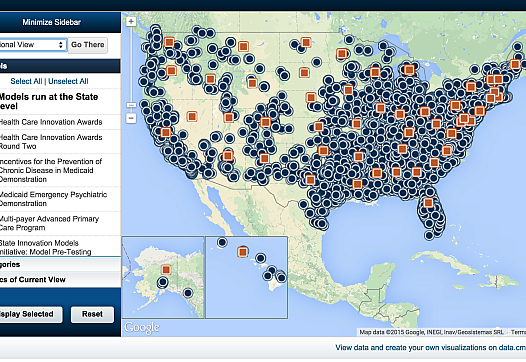
The old system of paying for health care may be broken, but is the future finally knocking on the door? And if so, what kinds of health care innovations will lead us forward to the promised land of lower costs and quality care? Our recent webinar took up these questions and more.

Medicare made more than $583 billion in payments in 2013. But, for one of the fastest rising areas of Medicare spending, the agency has no way of knowing whether all that money was spent wisely.

An innovative program allows elderly residents to remain in their own homes, rather than in a nursing home. At AltaMed's El Monte clinic, a 14-member interdisciplinary team coordinates each senior patient’s care, and vulnerable seniors are kept as busy and engaged as possible.

The 2015 California Health Journalism Fellowship kicked off with a wide-ranging conversation between Gerald Kominski of UCLA's Center for Health Policy Research and Anna Gorman of Kaiser Health News on the past and future of health reform.

The practice of physicians "self-referring" patients to facilities in which they or their families have a financial stake has dramatically increased in some specialties. The practice increases health costs for procedures and tests that are of questionable benefit to patients.

A series of reports has found that physicians who "self-refer" are following their financial interests and not always the best interests of their patients. The trend is driving up health care costs and potentially putting patients at risk from unnecessary services.