Denise’s Last Days
This story was undertaken as a project for the USC Center for Health Journalism’s 2022 National Fellowship.

Photo Illustration by Slate. Photos courtesy of Jackie Guzman.
About a year before her death, Denise Lerma began taking the steps she thought would save her life. First, she quit shooting heroin into her veins. Then she walked as far away from a lifetime of homelessness as her traumatized body and psyche could take her.
On her last day living in Lincoln Park, in Los Angeles, Lerma handed Louis, a friend living in the encampment, a pink balloon. It was her way of cheering him up.
Then she took her boyfriend Paul, who had been living with her in the tent across from the railroad tracks for years, to a Walmart, where she bought him a T-shirt. Afterward, she took him to the barber. She spent the last of her Social Security money that month getting him a shave and a haircut.
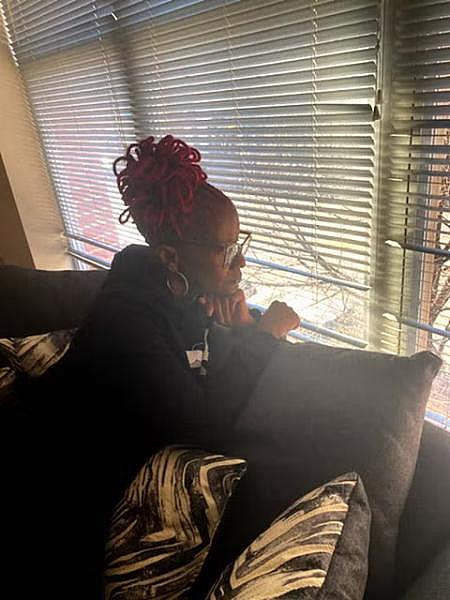
Known as a bit of a fashionista, Lerma took care of her appearance, styling her hair and, when she could, painting her nails. She adored wearing bright colors, particularly hot pink.
“You need to take better care of yourself,” Lerma admonished her boyfriend one last time. It was as if she was talking to herself as much as she was to him; there is no doubt that when she decided to leave that tent in Lincoln Park, she was walking toward a life that she wanted, perhaps for the first time, to live.
She walked inside their two-person tent to pack her bags. She had been nearly killed twice inside that tent—once by a drunk driver who careened off the street and plowed over her while she was sleeping, and once by a man who had run through the homeless encampment throwing lit torches at people’s sleeping bags and tents.
Those stories are just two of the obvious traumas of Lerma’s homelessness, the ones you could point to as life-threatening. But so much more had happened—particularly chronic traumas so inexorably linked to homelessness. For the unsheltered, these add up like microaggressions, so ubiquitous and condoned by society in their nature that they feel as ceaseless as the unending stretches of pavement Lerma traversed so carefully every day.
Yet even a mosquito bite, painful but bearable at first, if repeated enough times can create a state of such intolerability that the person under attack will eventually collapse. The trauma of homelessness, seen and unseen, is what killed Lerma—and it continues to prematurely end the lives of so many unsheltered people in America.
To begin to understand the unseen part of this story, consider the countless occasions when Lerma had waited for Uber drivers she had scheduled days in advance to take her to doctor appointments, her carefully tended hair swept back into a ponytail, her fingernails glossed with one of her favorite glitter colors; as soon as the drivers realized Lerma was homeless, they sped by. It happened so often that when they were asked to remember Denise, many painted this scene: Denise, walking ever so slowly because of the numbness and pain in her feet, leaning heavily into her metal cane for support as she heads across yet another parking lot to wait for a ride to an appointment.
Those missed appointments were much more than a personal affront. Their aftermath built up over time, and the domino effect of them debilitated her: They caused Lerma, who had advanced liver disease, to be labeled as “noncompliant” by her doctors. This meant she was relegated to the bottom of waiting lists for new appointments that took weeks, sometimes even months, to occur. That reality proved treacherous, said medical professionals who worked with Lerma: Unless she went to an emergency room in extreme distress, her advanced liver disease went unmonitored.
Lerma died on May 10, 2021, five days after telling friends and family that she had just learned that she had terminal liver cancer, a likely progression of the liver disease. She was 55.
Today, her death—and her life—serve as a clarion call for a new way of thinking about and treating the unfathomable experiences of people in situations like Lerma’s. The use of such a methodology could have helped prolong her life, perhaps even have saved it.
“It was hard to read through Denise’s medical charts and see the unnecessary suffering,” said Corinne Feldman, the co-founder of USC Street Medicine, a team of doctors, physician assistants, nurses, and other workers who care for people living on the streets. “And though it’s hard to point to any single person or event and say ‘There, that’s where the harm was inflicted,’ it is clear that there were so many times when we as a collective failed to give Denise the help she needed. The end of her life was a culmination of many missed opportunities.”
If there is a quintessential definition of what a lack of “trauma awareness” in our understanding of homelessness means, Feldman’s statements capture it: It is about our collective refusal to even acknowledge what life is actually like for this already severely marginalized population. This lack of awareness causes us to ignore the ways we—individuals as well as bureaucratic systems—could fill the gaping holes into which the unhoused suffer and fall, often to their deaths.
The life expectancies of the more than half a million people living on the streets and in shelters on any given night in this country are nearly 20 years less than those of their housed counterparts. Meanwhile, the number of people dying while unhoused has increased dramatically in the past five years, according to an analysis by the Guardian performed in conjunction with an academic expert at the University of Washington. The analysis examined 20 urban U.S. areas, discovering that deaths of people living without housing had shot up by 77 percent between 2015 and 2020.
It’s not just that the likelihood that you might die while unhoused is increasing—the number of unhoused people in the United States is going up, too. In 2022, rents increased at a rate unseen since 1986—the average rent for a one-bedroom apartment in Los Angeles is now $2,734—and shelters across the U.S have reported a startling uptick in the number of people looking for help, sometimes doubling and even tripling waitlists in the process. Two months ago, the new mayor of Los Angeles declared homelessness a state of emergency. “This is a matter of life and death,” she tweeted on Dec. 12. She is right—and the direct connection between an unhoused life and the ways it increases the risks of an early death is essential to understand, because we, as a society, could do something about it.
Denise Lerma died in the context of reversible but unhealed trauma. Her story is typical. In looking at what she often never received, we can see a different path for the hundreds of thousands who still live unhoused. We can see real hope.
On that last day that Lerma walked into the cramped orange and gray tent that she shared with her boyfriend, Paul Carrera, he said that she told him emphatically: “I’m leaving, and I’m not coming back.”
The couple had lived together in homelessness for nearly 10 years. But, Carrera said, “I knew I was never going to see her again.”
He thought Lerma was going to do what hurting animals do when it is their time to pass—isolate. Lerma never went back to their tent after that caring shopping spree for Carrera. But her departure wasn’t for the reason he assumed.

LA County Health Services registered nurse Darian Sumbingco administers the COVID vaccine to Denise Lerma, who was living unhoused near Lincoln Park in Los Angeles, on Thursday, Oct. 7, 2021. Credit: Al Seib/Los Angeles Times/Getty Images.
Lerma hadn’t left him to walk toward her death. She had left him to walk toward life. It was 2020, and she was ready to start a new life—without him. Without being surrounded by drugs and violence and the threat of death. Without the powerlessness of homelessness.
Lerma was Latina, but her nickname was “Huera,” Spanish slang for “white girl,” because of her light-colored skin. It was true that, in many ways, Lerma had been broken down. But her friends say she also had a quiet independence about her. When you told her “no,” she didn’t beg you to change your mind. She would take it upon herself to find another way.
Lerma wanted a life where she could have access to basics that give people the ability to regulate their lives: a toilet, a bed where she could sleep without fear of being murdered, a reliable source of food.
Those who tracked the next eight months of Lerma’s life included the medical professionals who were helping to care for her. They told me they watched Lerma become free of her addiction, then volunteer as a mentor for University of Southern California medical students who were learning how to work with the unhoused—feats she accomplished while going back and forth between hospitals for emergency care, a respite facility that cares for the unhoused, and the streets.
Corinne Feldman, the physician assistant who helps lead the USC Street Medicine team, and the team’s director, Brett Feldman, her husband, first began helping Lerma after Lerma was run over by the drunk driver as she was sleeping in her tent.

Denise Lerma comforts Paul Carrera after they received the COVID vaccine shots. Credit: Al Seib/Los Angeles Times/Getty Images.
Due to the severe, pre-existing nerve damage in Lerma’s feet, Lerma had mobility issues even before the driver rolled over her arm with his vehicle, Corinne Feldman said. But in the five days that she waited in her tent for help, Lerma developed ulcers on her legs, a result of her inability to move, bathe, or even change her clothes, Feldman said. Finally, as shown at 5:37 in this video from Invisible People, Lerma was lifted into an ambulance and taken to a hospital for treatment.
The Feldmans became well acquainted with Lerma months before that accident—but she had never asked for help for herself, only for her friends in the encampment.
“She would take us to people that she was worried about,” Brett Feldman said.
Her lack of focus on her own needs, even in the dire reality of homelessness, Feldman said, was something he sees a lot among the unhoused. It is often an internalization of society’s hatred of them, he explained. In response, unsheltered individuals can unconsciously employ a protective mechanism of “a kind of body and space dissociation,” and in that distancing from their own psyches, Feldman said, “they see what they are going through as not actually happening to them.”
Perhaps this is why so many unhoused people will tell you they are “fine” even when they are suffering physically and emotionally, Feldman concluded.
It’s a survival mechanism Lerma learned in childhood.
She grew up in a home where trauma was common, said her older sister, Jackie Guzman, who is three years her senior. Both of their parents were heroin addicts, and it seemed that Lerma was born addicted. She was a sickly child, always catching colds and coming down with infections, Guzman said. It was a regular occurrence for the children to hear their father beat their mother as the sisters hid in a nearby closet. It was also common to see the police in their home.
“There were so many people in and out of our homes buying drugs, selling drugs,” Guzman said.
In that chaos, her little sister was molested by a man in his 60s, someone the children knew as “Uncle Tom,” though he wasn’t related to them. After witnessing the molestation, Denise’s older brother got an ax and chopped into the man’s head, Guzman said, and there was blood everywhere. The man survived—and he was even brazen enough to come back with gauze wrapped around his head from the ax wound. But he never hurt Denise again.
Such adversities in childhood are called Adverse Childhood Experiences, or ACEs, a term coined by researchers in a seminal study of 13,000 people from 1995 to 1997 at Kaiser Permanente’s San Diego Health Appraisal Clinic. The study included a survey mailed to more than 13,000 adults and found a direct relationship between the number of ACEs a person experiences and the decreased chances of that individual having the ability to thrive, let alone live a normal, healthy, long life.
When referring to psychological pain, the term trauma is defined as one possible outcome of exposure to adversity, according to a 2019 article by Child Trends, a national organization that focuses exclusively on improving the lives of children. Concurrently, toxic stress is seen as a reaction to childhood adversities that can over-activate a child’s stress response system, wearing down the body and brain. The love and guidance of an appropriate caregiver can disrupt this cycle. And most children are able to recover when they have those kinds of supports, studies have shown. In Lerma’s case, there was an elderly neighbor who took her under his wing, cooking her meals and, when she was old enough, teaching her how to drive. But it wasn’t enough for Lerma to overcome her sense of being unloved by her family of origin.
“We failed Denise Lerma when she was a child,” Diederik Wolsak told me. “No one said, ‘Denise, the fact that your mom and dad are addicts has nothing to do with you.’ ”
Wolsak knows a lot about the subject: He’s a trauma-aware counselor who survived three years in World War II concentration camps as a child, and has been conducting workshops worldwide for more than 30 years. Wolsak’s life work helps people transform negative core beliefs that formed during childhood and that have persistently affected their lives—he runs a program, Choose Again, that serves thousands of Americans. His work has shown him that without intervention, a child in Denise Lerma’s position inevitably thinks, “If my parents are gloriously happy, I am a wonderful person. But if my parents are both heroin addicts, then I must be an absolute complete waste of time. I must have no rights at all.”
By the time Lerma was 17, she had dropped out of high school because she couldn’t focus on her studies, her sister said. Then she became homeless. The men she wound up with were substance abusers, Guzman said, people her sister had difficulty breaking free from because she thought she was supposed to do what she couldn’t with her own parents: save them from their addictions.
Meanwhile, the trauma Lerma was experiencing in homelessness was continual, Guzman noted. Her sister was robbed. Her sister was stabbed. You name it, it happened.
Lerma relied on drugs to self-medicate, and she dramatically escalated those efforts when, because of her inability to care for them, the seven children she eventually had were each taken from her by authorities, Guzman told me.
There were counselors who tried to help Lerma, but their efforts couldn’t reverse her long history, according to Guzman: “By that time, Denise had serious trust issues. She’d been violated. She pretty much slept with one eye open on Skid Row for at least 10 years. She wouldn’t—couldn’t—just open up to people.”
She had become a woman who held her head low, averted her eyes; a woman with the reputation of being an intensely private person, especially when it came to disclosing the details of her substance abuse and homelessness.
“She felt judged,” said Pooja Bhalla, co-chief executive officer of Illumination Foundation. Lerma came and went from Illumination Foundation for a period of about two to three years, Bhalla said, in the later part of her life.
Illumination Foundation tries to do things a little bit differently. Because so many of the people they work with have such severe histories of trauma, they focus on training their staff in a way that takes this into account, one of the components of trauma-awareness.
At its core, trauma-awareness means that a person’s experiences are recognized in a way that simultaneously honors the resilience that has allowed that individual to survive. This recognition meets that inner strength with resources that shore it up and sustain it.
Illumination Foundation not only uses trauma-aware practices, they offer recuperative care centers for medically vulnerable people who have left hospitals and are facing homelessness. “It took her a while to engage with our case managers because of trust and safety issues,” Bhalla said.
Lerma’s story shows, strikingly, the difference between current standards of care and trauma-aware care, because it was while Lerma was working with Illumination Foundation—and the USC Street Medicine team—that things first started to change for her. This was in September 2021, after the car ran over her in the tent.
By that time, her liver disease was quite advanced, said Corinne Feldman, the physician assistant who heads the USC team. Making matters worse was the fact that Lerma had not been taking her liver medications for more than a year. The reason, Feldman said, was crushing: Lerma had been prescribed lactulose, a medication that is common for liver disease, but that caused severe diarrhea. Since Lerma was often living on the streets, she didn’t have regular access to a bathroom where she could clean herself. She was told she ought to take a medicine that was supposed to make her feel better, but she knew she would end up having chronic diarrhea in a situation where she would face the humiliation of soiling herself without a place to wash her clothes afterward.
It is not known whether Lerma told her doctors why she wouldn’t take the medication. A question naturally arises about Lerma’s treatment: How could the doctors take into consideration the fact that Lerma was unhoused if Lerma didn’t tell them?
It’s an understandable question. But the answers are understandable, too: Because she didn’t want to. Because she almost couldn’t bear to. Because she wasn’t sure there would be another option, and she felt like she was already too much of a burden on the doctors helping her manage her disease.
Here is where why trauma-aware training can help: It puts the onus of gathering sensitive information squarely on the care provider, said Bobby Watts, chief executive officer of the National Health Care for the Homeless Council.
“We know that, because of the shame involved with homelessness, that if they ask, ’Are you homeless?’ people will say ‘No,’ ” he said. “But if we ask, ‘Where did you sleep last night?’ then you start to get some real information.”
Without trauma-aware training on how to ascertain a person’s housing status, the resulting failure to sensitively explore, document, and record homelessness during treatment protocols means that whatever care is provided often proves ineffective, Watts said. It’s such a simple thing, to shift the question a doctor asks, but the consequences for people’s lives can be enormous.
If and when the hurdle of disclosure is overcome, another equally insidious barricade to resources and care for the unhoused remains: Doctors still don’t trust them.
For Lerma, this looked like notes in medical charts that talked about how certain medical interventions would be complicated by a social history of “noncompliance” and “drug abuse,” Feldman told me. Maddeningly, those notes were made even after Lerma had become sober.
The wider societal context in which Lerma sought help is that of an institutional bias against already marginalized individuals. A 2021 Journal of the American Medical Association article on “stigmatizing language” used in medical records by physicians reported that “disapproval, discrediting, and stereotyping” words influenced care. “Implicit bias is the automatic activation of stereotypes, which may override deliberate thought and influence one’s judgment in unintentional and unrecognized ways,” the article states. Meanwhile, the findings of the study concluded that “Although often not explicit, this language could potentially transmit bias” and lead to lower-quality care, the article said.
Feldman estimates that she and her team advocated for Lerma across medical and homeless shelter systems at least a dozen times in the eight months they actively worked with her. They went with Lerma to the hospital, and they ironed out transportation details with various shelter staff. They even stood on street corners and waited for Uber drivers to arrive: “Then we’d do a bait-and-switch and say to the driver who had just pulled up, ‘Let me get my friend.’ Then we would bring Denise over,” said Brett Feldman; it was too late for the driver to cancel.
By the time the USC medical students met Lerma, she had become so quietly guarded that she could appear overly grateful when shown the smallest of social niceties. “She wasn’t used to basic kindness,” said Kimberly Su, a second-year medical student who helped Lerma go to doctor appointments. “Once, all I did was listen to Denise tell me about her day and she cried with appreciation. It happened on multiple occasions.”
About a year before her death, Denise Lerma began taking the steps she thought would save her life. First, she quit shooting heroin into her veins. Then she walked as far away from a lifetime of homelessness as her traumatized body and psyche could take her.
On her last day living in Lincoln Park, in Los Angeles, Lerma handed Louis, a friend living in the encampment, a pink balloon. It was her way of cheering him up.
Then she took her boyfriend Paul, who had been living with her in the tent across from the railroad tracks for years, to a Walmart, where she bought him a T-shirt. Afterward, she took him to the barber. She spent the last of her Social Security money that month getting him a shave and a haircut.
Known as a bit of a fashionista, Lerma took care of her appearance, styling her hair and, when she could, painting her nails. She adored wearing bright colors, particularly hot pink.
“You need to take better care of yourself,” Lerma admonished her boyfriend one last time. It was as if she was talking to herself as much as she was to him; there is no doubt that when she decided to leave that tent in Lincoln Park, she was walking toward a life that she wanted, perhaps for the first time, to live.
She walked inside their two-person tent to pack her bags. She had been nearly killed twice inside that tent—once by a drunk driver who careened off the street and plowed over her while she was sleeping, and once by a man who had run through the homeless encampment throwing lit torches at people’s sleeping bags and tents.
Those stories are just two of the obvious traumas of Lerma’s homelessness, the ones you could point to as life-threatening. But so much more had happened—particularly chronic traumas so inexorably linked to homelessness. For the unsheltered, these add up like microaggressions, so ubiquitous and condoned by society in their nature that they feel as ceaseless as the unending stretches of pavement Lerma traversed so carefully every day.
Yet even a mosquito bite, painful but bearable at first, if repeated enough times can create a state of such intolerability that the person under attack will eventually collapse. The trauma of homelessness, seen and unseen, is what killed Lerma—and it continues to prematurely end the lives of so many unsheltered people in America.
To begin to understand the unseen part of this story, consider the countless occasions when Lerma had waited for Uber drivers she had scheduled days in advance to take her to doctor appointments, her carefully tended hair swept back into a ponytail, her fingernails glossed with one of her favorite glitter colors; as soon as the drivers realized Lerma was homeless, they sped by. It happened so often that when they were asked to remember Denise, many painted this scene: Denise, walking ever so slowly because of the numbness and pain in her feet, leaning heavily into her metal cane for support as she heads across yet another parking lot to wait for a ride to an appointment.
Those missed appointments were much more than a personal affront. Their aftermath built up over time, and the domino effect of them debilitated her: They caused Lerma, who had advanced liver disease, to be labeled as “noncompliant” by her doctors. This meant she was relegated to the bottom of waiting lists for new appointments that took weeks, sometimes even months, to occur. That reality proved treacherous, said medical professionals who worked with Lerma: Unless she went to an emergency room in extreme distress, her advanced liver disease went unmonitored.
Lerma died on May 10, 2021, five days after telling friends and family that she had just learned that she had terminal liver cancer, a likely progression of the liver disease. She was 55.
Today, her death—and her life—serve as a clarion call for a new way of thinking about and treating the unfathomable experiences of people in situations like Lerma’s. The use of such a methodology could have helped prolong her life, perhaps even have saved it.
“It was hard to read through Denise’s medical charts and see the unnecessary suffering,” said Corinne Feldman, the co-founder of USC Street Medicine, a team of doctors, physician assistants, nurses, and other workers who care for people living on the streets. “And though it’s hard to point to any single person or event and say ‘There, that’s where the harm was inflicted,’ it is clear that there were so many times when we as a collective failed to give Denise the help she needed. The end of her life was a culmination of many missed opportunities.”
Deaths of people living without housing shot up by 77 percent between 2015 and 2020.
If there is a quintessential definition of what a lack of “trauma awareness” in our understanding of homelessness means, Feldman’s statements capture it: It is about our collective refusal to even acknowledge what life is actually like for this already severely marginalized population. This lack of awareness causes us to ignore the ways we—individuals as well as bureaucratic systems—could fill the gaping holes into which the unhoused suffer and fall, often to their deaths.
The life expectancies of the more than half a million people living on the streets and in shelters on any given night in this country are nearly 20 years less than those of their housed counterparts. Meanwhile, the number of people dying while unhoused has increased dramatically in the past five years, according to an analysis by the Guardian performed in conjunction with an academic expert at the University of Washington. The analysis examined 20 urban U.S. areas, discovering that deaths of people living without housing had shot up by 77 percent between 2015 and 2020.
It’s not just that the likelihood that you might die while unhoused is increasing—the number of unhoused people in the United States is going up, too. In 2022, rents increased at a rate unseen since 1986—the average rent for a one-bedroom apartment in Los Angeles is now $2,734—and shelters across the U.S have reported a startling uptick in the number of people looking for help, sometimes doubling and even tripling waitlists in the process. Two months ago, the new mayor of Los Angeles declared homelessness a state of emergency. “This is a matter of life and death,” she tweeted on Dec. 12. She is right—and the direct connection between an unhoused life and the ways it increases the risks of an early death is essential to understand, because we, as a society, could do something about it.
Denise Lerma died in the context of reversible but unhealed trauma. Her story is typical. In looking at what she often never received, we can see a different path for the hundreds of thousands who still live unhoused. We can see real hope.
On that last day that Lerma walked into the cramped orange and gray tent that she shared with her boyfriend, Paul Carrera, he said that she told him emphatically: “I’m leaving, and I’m not coming back.”
The couple had lived together in homelessness for nearly 10 years. But, Carrera said, “I knew I was never going to see her again.”
He thought Lerma was going to do what hurting animals do when it is their time to pass—isolate. Lerma never went back to their tent after that caring shopping spree for Carrera. But her departure wasn’t for the reason he assumed.
Lerma hadn’t left him to walk toward her death. She had left him to walk toward life. It was 2020, and she was ready to start a new life—without him. Without being surrounded by drugs and violence and the threat of death. Without the powerlessness of homelessness.
Lerma was Latina, but her nickname was “Huera,” Spanish slang for “white girl,” because of her light-colored skin. It was true that, in many ways, Lerma had been broken down. But her friends say she also had a quiet independence about her. When you told her “no,” she didn’t beg you to change your mind. She would take it upon herself to find another way.
Lerma wanted a life where she could have access to basics that give people the ability to regulate their lives: a toilet, a bed where she could sleep without fear of being murdered, a reliable source of food.
Those who tracked the next eight months of Lerma’s life included the medical professionals who were helping to care for her. They told me they watched Lerma become free of her addiction, then volunteer as a mentor for University of Southern California medical students who were learning how to work with the unhoused—feats she accomplished while going back and forth between hospitals for emergency care, a respite facility that cares for the unhoused, and the streets.
Corinne Feldman, the physician assistant who helps lead the USC Street Medicine team, and the team’s director, Brett Feldman, her husband, first began helping Lerma after Lerma was run over by the drunk driver as she was sleeping in her tent.
Denise Lerma comforts Paul Carrera after they received the COVID vaccine shots. Credit: Al Seib/Los Angeles Times/Getty Images.
Due to the severe, pre-existing nerve damage in Lerma’s feet, Lerma had mobility issues even before the driver rolled over her arm with his vehicle, Corinne Feldman said. But in the five days that she waited in her tent for help, Lerma developed ulcers on her legs, a result of her inability to move, bathe, or even change her clothes, Feldman said. Finally, as shown at 5:37 in this video from Invisible People, Lerma was lifted into an ambulance and taken to a hospital for treatment.
The Feldmans became well acquainted with Lerma months before that accident—but she had never asked for help for herself, only for her friends in the encampment.
“She would take us to people that she was worried about,” Brett Feldman said.
Her lack of focus on her own needs, even in the dire reality of homelessness, Feldman said, was something he sees a lot among the unhoused. It is often an internalization of society’s hatred of them, he explained. In response, unsheltered individuals can unconsciously employ a protective mechanism of “a kind of body and space dissociation,” and in that distancing from their own psyches, Feldman said, “they see what they are going through as not actually happening to them.”
Perhaps this is why so many unhoused people will tell you they are “fine” even when they are suffering physically and emotionally, Feldman concluded.
It’s a survival mechanism Lerma learned in childhood.
She grew up in a home where trauma was common, said her older sister, Jackie Guzman, who is three years her senior. Both of their parents were heroin addicts, and it seemed that Lerma was born addicted. She was a sickly child, always catching colds and coming down with infections, Guzman said. It was a regular occurrence for the children to hear their father beat their mother as the sisters hid in a nearby closet. It was also common to see the police in their home.
“There were so many people in and out of our homes buying drugs, selling drugs,” Guzman said.
In that chaos, her little sister was molested by a man in his 60s, someone the children knew as “Uncle Tom,” though he wasn’t related to them. After witnessing the molestation, Denise’s older brother got an ax and chopped into the man’s head, Guzman said, and there was blood everywhere. The man survived—and he was even brazen enough to come back with gauze wrapped around his head from the ax wound. But he never hurt Denise again.
Such adversities in childhood are called Adverse Childhood Experiences, or ACEs, a term coined by researchers in a seminal study of 13,000 people from 1995 to 1997 at Kaiser Permanente’s San Diego Health Appraisal Clinic. The study included a survey mailed to more than 13,000 adults and found a direct relationship between the number of ACEs a person experiences and the decreased chances of that individual having the ability to thrive, let alone live a normal, healthy, long life.
When referring to psychological pain, the term trauma is defined as one possible outcome of exposure to adversity, according to a 2019 article by Child Trends, a national organization that focuses exclusively on improving the lives of children. Concurrently, toxic stress is seen as a reaction to childhood adversities that can over-activate a child’s stress response system, wearing down the body and brain. The love and guidance of an appropriate caregiver can disrupt this cycle. And most children are able to recover when they have those kinds of supports, studies have shown. In Lerma’s case, there was an elderly neighbor who took her under his wing, cooking her meals and, when she was old enough, teaching her how to drive. But it wasn’t enough for Lerma to overcome her sense of being unloved by her family of origin.
“We failed Denise Lerma when she was a child,” Diederik Wolsak told me. “No one said, ‘Denise, the fact that your mom and dad are addicts has nothing to do with you.’ ”
Her sister was robbed. Her sister was stabbed. You name it, it happened.
Wolsak knows a lot about the subject: He’s a trauma-aware counselor who survived three years in World War II concentration camps as a child, and has been conducting workshops worldwide for more than 30 years. Wolsak’s life work helps people transform negative core beliefs that formed during childhood and that have persistently affected their lives—he runs a program, Choose Again, that serves thousands of Americans. His work has shown him that without intervention, a child in Denise Lerma’s position inevitably thinks, “If my parents are gloriously happy, I am a wonderful person. But if my parents are both heroin addicts, then I must be an absolute complete waste of time. I must have no rights at all.”
By the time Lerma was 17, she had dropped out of high school because she couldn’t focus on her studies, her sister said. Then she became homeless. The men she wound up with were substance abusers, Guzman said, people her sister had difficulty breaking free from because she thought she was supposed to do what she couldn’t with her own parents: save them from their addictions.
Meanwhile, the trauma Lerma was experiencing in homelessness was continual, Guzman noted. Her sister was robbed. Her sister was stabbed. You name it, it happened.
Lerma relied on drugs to self-medicate, and she dramatically escalated those efforts when, because of her inability to care for them, the seven children she eventually had were each taken from her by authorities, Guzman told me.
There were counselors who tried to help Lerma, but their efforts couldn’t reverse her long history, according to Guzman: “By that time, Denise had serious trust issues. She’d been violated. She pretty much slept with one eye open on Skid Row for at least 10 years. She wouldn’t—couldn’t—just open up to people.”
She had become a woman who held her head low, averted her eyes; a woman with the reputation of being an intensely private person, especially when it came to disclosing the details of her substance abuse and homelessness.
“She felt judged,” said Pooja Bhalla, co-chief executive officer of Illumination Foundation. Lerma came and went from Illumination Foundation for a period of about two to three years, Bhalla said, in the later part of her life.
Illumination Foundation tries to do things a little bit differently. Because so many of the people they work with have such severe histories of trauma, they focus on training their staff in a way that takes this into account, one of the components of trauma-awareness.
At its core, trauma-awareness means that a person’s experiences are recognized in a way that simultaneously honors the resilience that has allowed that individual to survive. This recognition meets that inner strength with resources that shore it up and sustain it.
Illumination Foundation not only uses trauma-aware practices, they offer recuperative care centers for medically vulnerable people who have left hospitals and are facing homelessness. “It took her a while to engage with our case managers because of trust and safety issues,” Bhalla said.
Lerma’s story shows, strikingly, the difference between current standards of care and trauma-aware care, because it was while Lerma was working with Illumination Foundation—and the USC Street Medicine team—that things first started to change for her. This was in September 2021, after the car ran over her in the tent.
By that time, her liver disease was quite advanced, said Corinne Feldman, the physician assistant who heads the USC team. Making matters worse was the fact that Lerma had not been taking her liver medications for more than a year. The reason, Feldman said, was crushing: Lerma had been prescribed lactulose, a medication that is common for liver disease, but that caused severe diarrhea. Since Lerma was often living on the streets, she didn’t have regular access to a bathroom where she could clean herself. She was told she ought to take a medicine that was supposed to make her feel better, but she knew she would end up having chronic diarrhea in a situation where she would face the humiliation of soiling herself without a place to wash her clothes afterward.
It is not known whether Lerma told her doctors why she wouldn’t take the medication. A question naturally arises about Lerma’s treatment: How could the doctors take into consideration the fact that Lerma was unhoused if Lerma didn’t tell them?
It’s an understandable question. But the answers are understandable, too: Because she didn’t want to. Because she almost couldn’t bear to. Because she wasn’t sure there would be another option, and she felt like she was already too much of a burden on the doctors helping her manage her disease.
Here is where why trauma-aware training can help: It puts the onus of gathering sensitive information squarely on the care provider, said Bobby Watts, chief executive officer of the National Health Care for the Homeless Council.
“We know that, because of the shame involved with homelessness, that if they ask, ’Are you homeless?’ people will say ‘No,’ ” he said. “But if we ask, ‘Where did you sleep last night?’ then you start to get some real information.”
Without trauma-aware training on how to ascertain a person’s housing status, the resulting failure to sensitively explore, document, and record homelessness during treatment protocols means that whatever care is provided often proves ineffective, Watts said. It’s such a simple thing, to shift the question a doctor asks, but the consequences for people’s lives can be enormous.
If and when the hurdle of disclosure is overcome, another equally insidious barricade to resources and care for the unhoused remains: Doctors still don’t trust them.
For Lerma, this looked like notes in medical charts that talked about how certain medical interventions would be complicated by a social history of “noncompliance” and “drug abuse,” Feldman told me. Maddeningly, those notes were made even after Lerma had become sober.
The wider societal context in which Lerma sought help is that of an institutional bias against already marginalized individuals. A 2021 Journal of the American Medical Association article on “stigmatizing language” used in medical records by physicians reported that “disapproval, discrediting, and stereotyping” words influenced care. “Implicit bias is the automatic activation of stereotypes, which may override deliberate thought and influence one’s judgment in unintentional and unrecognized ways,” the article states. Meanwhile, the findings of the study concluded that “Although often not explicit, this language could potentially transmit bias” and lead to lower-quality care, the article said.
Feldman estimates that she and her team advocated for Lerma across medical and homeless shelter systems at least a dozen times in the eight months they actively worked with her. They went with Lerma to the hospital, and they ironed out transportation details with various shelter staff. They even stood on street corners and waited for Uber drivers to arrive: “Then we’d do a bait-and-switch and say to the driver who had just pulled up, ‘Let me get my friend.’ Then we would bring Denise over,” said Brett Feldman; it was too late for the driver to cancel.
By the time the USC medical students met Lerma, she had become so quietly guarded that she could appear overly grateful when shown the smallest of social niceties. “She wasn’t used to basic kindness,” said Kimberly Su, a second-year medical student who helped Lerma go to doctor appointments. “Once, all I did was listen to Denise tell me about her day and she cried with appreciation. It happened on multiple occasions.”
What can trauma-aware care look like on the streets? Corinne Feldman said that it starts with emphatic concern: “Rather than blaming Denise—saying ‘Patient remains noncompliant,’ for example, you ask the question, ‘How can we support you, Denise?’ ”
One of the most overlooked aspects of the trauma of homelessness is the limbic-system impairment that can occur. The limbic system is a complex set of structures in the brain widely known to be associated with emotion, learning, memory, and the body’s stress response. In trauma, and especially with chronic trauma that is not treated in a timely manner, the limbic system can get stuck in one of the classic trauma responses of “flight, fight, or freeze.”
Ongoing trauma stressors can lead to an exhaustive list of symptoms including depression, substance abuse, dissociation, health problems, and post-traumatic stress disorder. In the words of researchers, “chronic stress induces changes” in “neuronal systems at several levels, inducing alterations in size of brain nuclei.” In other words, it literally alters the brain.
If left untreated, symptoms can lead to chronic inflammation, the origin of many life-threatening conditions including heart disease, cancer, diabetes, and rheumatoid arthritis, according to the Cleveland Clinic.
Even if a person doesn’t have risk factors associated with developing those conditions, that person is more likely to develop them if they have a high number of Adverse Childhood Experiences or if they have dealt with a lot of chronic stress.
Lerma’s symptoms were largely untreated. Like an estimated 92 percent of unhoused people, she didn’t have a primary health care physician until the USC Street Medicine team took on this role in 2021. And underlying our society’s refusal to fix this problem is a shaming and blaming of the homeless—particularly through stereotypes that the unhoused are “lazy,” “drug addicted,” or “crazy”—foisting the onus of solving the problem onto the people suffering from it. The demographics of homelessness show how systemic racism deepens this stigma: Black people comprise 40 percent of the unsheltered population while comprising only 13 percent of the general population. Hispanic people make up a share of the population approximately equal to their share of the general population, and white people are significantly underrepresented.
Koumba Yasin says people assumed she wanted to be unhoused. “I ate out of trash cans sometimes, and I smelled really, really bad,” Yasin, a Black woman who lives in Baltimore, told me. “Because along with my depression and being homeless, I wasn’t showering.”
Now 52, she recounts that after a man raped her while she was experiencing homelessness—she was 26 at the time—two white male detectives from a crime unit asked her what she had been wearing, and whether she had been promiscuous. Their interrogation worsened Yasin’s suspicion and bad feelings toward the system and people in general, she said. She didn’t get any of the care she needed to recover after the rape. Instead, “I went back to the streets and getting high because I didn’t want to feel what I was feeling,” Yasin remembered. “It was like I had a hatred of the system—a big hatred.”
A report published by the Substance Abuse and Mental Health Services Administration suggests the greater the acculturation of an unhoused person back into society after trauma, the lower the levels of PTSD symptoms will be. But for the next 26 years, Yasin remained an outlier, stuck in the cycle of incarceration and homelessness. For her, that looked like stealing goods from the mall to pay for drugs to self-medicate her pain, and then repeatedly going to Jessup Correctional Institution for doing so.
Koumba Yasin. Photo by Buffy Buchanan
The door between homelessness and prison revolves at a high speed—a 2018 report from the Prison Policy Initiative shows that, due to the criminalization of unsheltered people, the unhoused are 10 times more likely to be incarcerated than the housed.
But things began to change for Yasin in 2020. She began living in a hotel that had been converted into a shelter for unhoused women, and began working with a counselor and other trauma-aware health care professionals assembled by Health Care for the Homeless in Maryland. It was this stability—the ability to begin to feel safe and access everything from food to mental health care—that allowed Yasin to start to heal.
Her voice filled with gratitude as she talked about a counselor whose office had soothing music and walls with placards with simple phrases like “You are worthy” and “You come from a place of greatness.”
Instead of telling Yasin what to do—a misstep in trauma-aware care—the counselor invited Yasin to sit down and have a cup of tea. “She always told me that what happened wasn’t my fault, and that I’m beautiful,” Yasin said. She had grown up being told she “wasn’t any good” and “would never amount to anything,” she told me, and those words dug deep grooves in her mind, trenches she couldn’t climb out of by herself.
Despite the damage that trauma can cause, there is also the fact of neuroplasticity: the ability of the brain to reorganize its synaptic connections and build healthier neural pathways. A foundation of this transformation is for a person to feel—and to be—safe.
In the early winter of 2020, Yasin moved out of the converted hotel that is now the Pinderhughes Women’s Shelter and into permanent, rapid re-housing paid for by Health Care for the Homeless. Now she’s in a government-subsidized one-bedroom apartment across the street from the Hippodrome Theatre in downtown Baltimore, an area that is in the midst of gentrification, which makes Yasin feel lucky to live there.
She showed me around her immaculately kept apartment during our Zoom interview. There’s the double-stacked washer and dryer, the sparkling white bathroom, the modern gray couch with matching black-and-white pillows.
“I’m moving forward,” Yasin said. “It feels amazing to even have survived these traumas—mentally, spiritually, and emotionally.” Yasin now works as a peer at Nuwave Health Services, a treatment center for people overcoming addiction, many of them formerly unhoused. She feels lucky “to be in a position to be working where I’m working and dealing with women who have come from some of the same traumas as me.”
Yasin is an artist and a poet. She said she thanks God for sustaining her through what, at the time, felt like inescapable challenges. And she also acknowledged her first conversation with a trauma-aware counselor at that hotel as being life-saving.
Said Yasin, “She spoke life into me.”
The last days of Denise Lerma’s life were symbolic of the 55 years preceding it: She died buried amid an avalanche of the unacknowledged traumas so irrevocably linked to the unhoused in America.
On May 5, 2021, Lerma texted the Street Medicine team, telling them that she had just heard from doctors that she had liver cancer, “and it’s really bad.” She went into one of Illumination Foundation’s recuperative care centers.

Denise with Street Medicine team nurse Dulce, shortly before Denise died. Courtesy of the USC Street Medicine team
On May 7, 2021, records from Illumination Foundation show that Lerma approached staff in the medication room and stated that on a scale of 1-10, she was at a 10 in terms of pain. She wasn’t given any more medication, because two hours previously, she had already received her 12-hour dose of oxycodone, an opioid prescribed for pain. A woman who was living at the center at the time said Lerma called her sobbing because of the pain.
At 11:55 p.m., Lerma requested to return to PIH Health Whittier Hospital in Los Angeles. Shortly after her arrival at the hospital, Guzman—Lerma’s sister—says she received a call from a doctor who asked to induce Lerma into a coma, due to the pain Lerma was experiencing.
Guzman asked the doctor to wait, telling them that she wanted her sister to hear her tell her that she loved her one last time, and that she was already driving from Las Vegas. She doesn’t know what happened in between. She just knows her sister died while she was on Interstate 605 in California, less than an hour away from the hospital.
The causes of death listed on Lerma’s death certificate, when translated through the language of trauma-awareness, unfold like a chronological summary of the continual wounding that had engulfed her life.
Alcoholic cirrhosis of the liver.
Self-medication of trauma that eventually resulted in advanced liver disease.
Multifocal hepatocellular carcinoma. A cancer of the liver that, when caught early, “can mean successful treatment with surgery or a liver transplant,” according to the Cleveland Clinic.
For all the reasons detailed in this story, Lerma did not know she had a deadly cancer until five days before she died.
Mesenteric venous thrombosis. A blood clot in one or more of the major veins that drains blood from the intestines—“the higher your cancer stage, the greater your risk for a blood clot,” say the Centers for Disease Control and Prevention.
A trauma that escalated to unstoppable proportions.
And finally, hypovolemic shock, a critical condition involving severe blood or other fluid loss that causes the heart to be unable to pump blood to the body.
The last trauma to Lerma’s body.
“Now I have to live with the fact that my sister died in pain,” Guzman said. “How am I supposed to do that? Can you tell me that?”
**
Correction, Feb. 21, 2023: The original version of this piece misstated the year of Denise Lerma’s death; it was 2022, not 2021.
[This article was originally published by SLATE.]
Did you like this story? Your support means a lot! Your tax-deductible donation will advance our mission of supporting journalism as a catalyst for change.
